- J-STAGEトップ
- /
- 日本口腔科学会雑誌
- /
- 70 巻 (2021) 4 号
- /
- 書誌
-
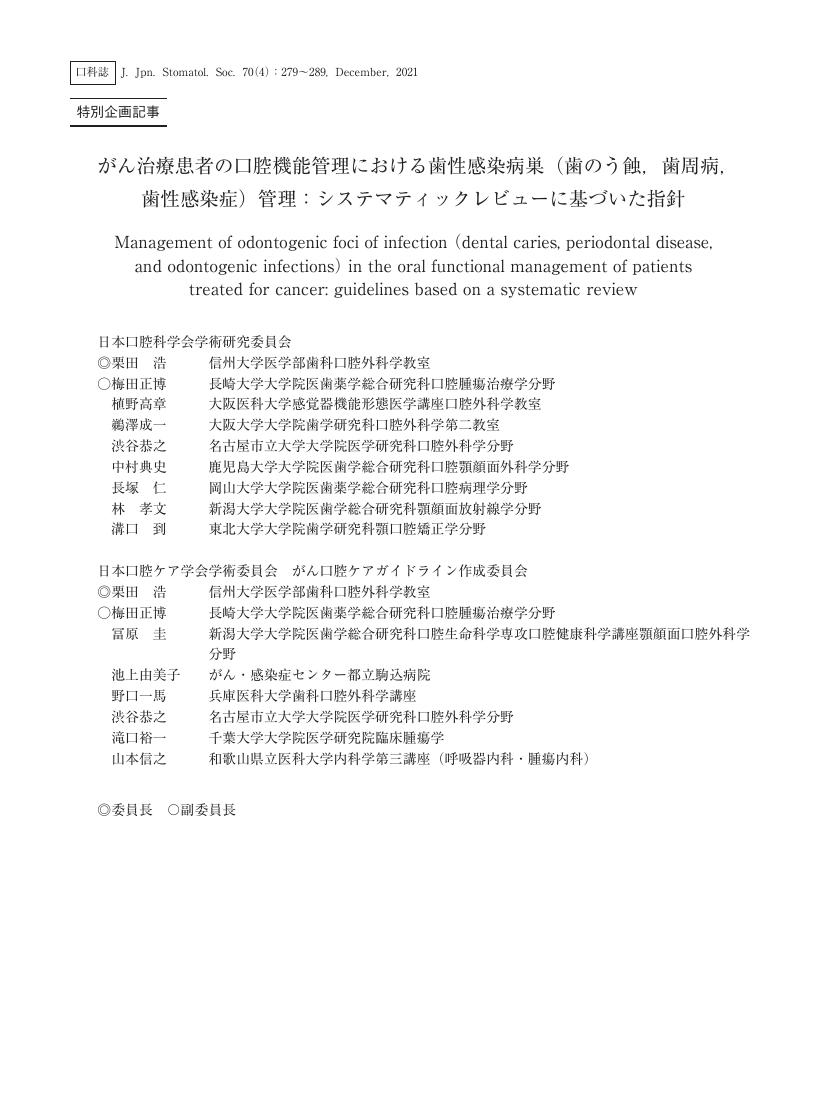
栗田 浩
日本口腔科学会学術研究委員会 日本口腔ケア学会学術委員会 がん口腔ケアガイドライン作成委員会 信州大学医学部歯科口腔外科学教室
-
梅田 正博
日本口腔科学会学術研究委員会 日本口腔ケア学会学術委員会 がん口腔ケアガイドライン作成委員会 長崎大学大学院医歯薬学総合研究科口腔腫瘍治療学分野
-
植野 高章
日本口腔科学会学術研究委員会 大阪医科大学感覚器機能形態医学講座口腔外科学教室
-
鵜澤 成一
日本口腔科学会学術研究委員会 大阪大学大学院歯学研究科口腔外科学第二教室
-
渋谷 恭之
日本口腔科学会学術研究委員会 日本口腔ケア学会学術委員会 がん口腔ケアガイドライン作成委員会 名古屋市立大学大学院医学研究科口腔外科学分野
-
中村 典史
日本口腔科学会学術研究委員会 鹿児島大学大学院医歯学総合研究科口腔顎顔面外科学分野
-
長塚 仁
日本口腔科学会学術研究委員会 岡山大学大学院医歯薬学総合研究科口腔病理学分野
-
林 孝文
日本口腔科学会学術研究委員会 新潟大学大学院医歯学総合研究科顎顔面放射線学分野
-
溝口 到
日本口腔科学会学術研究委員会 東北大学大学院歯学研究科顎口腔矯正学分野
-
冨原 圭
日本口腔ケア学会学術委員会 がん口腔ケアガイドライン作成委員会 新潟大学大学院医歯学総合研究科口腔生命科学専攻口腔健康科学講座顎顔面口腔外科学分野
-
池上 由美子
日本口腔ケア学会学術委員会 がん口腔ケアガイドライン作成委員会 がん・感染症センター都立駒込病院
-
野口 一馬
日本口腔ケア学会学術委員会 がん口腔ケアガイドライン作成委員会 兵庫医科大学歯科口腔外科学講座
-
滝口 裕一
日本口腔ケア学会学術委員会 がん口腔ケアガイドライン作成委員会 千葉大学大学院医学研究院臨床腫瘍学
-
山本 信之
日本口腔ケア学会学術委員会 がん口腔ケアガイドライン作成委員会 和歌山県立医科大学内科学第三講座(呼吸器内科・腫瘍内科)
2021 年 70 巻 4 号 p. 279-289
- 発行日: 2021 年 受付日: - J-STAGE公開日: 2021/12/25 受理日: - 早期公開日: - 改訂日: -
(EndNote、Reference Manager、ProCite、RefWorksとの互換性あり)
(BibDesk、LaTeXとの互換性あり)