Abstract
The currently used diagnostic criteria for acute pancreatitis in Japan are presentation with at least two of the following three manifestations: (1) acute abdominal pain and tenderness in the upper abdomen; (2) elevated levels of pancreatic enzyme in the blood, urine, or ascitic fluid; and (3) abnormal imaging findings in the pancreas associated with acute pancreatitis. When a diagnosis is made on this basis, other pancreatic diseases and acute abdomen can be ruled out. The purpose of this article is to review the conventional criteria and, in particular, the various methods of diagnosis based on pancreatic enzyme values, with the aim of improving the quality of diagnosis of acute pancreatitis and formulating common internationally agreed criteria. The review considers the following recommendations:
— Better even than the total blood amylase level, the blood lipase level is the best pancreatic enzyme for the diagnosis of acute pancreatitis and its differentiation from other diseases.
— A pivotal factor in the diagnosis of acute pancreatitis is identifying an increase in pancreatic enzymes in the blood.
— Ultrasonography (US) is also one of the procedures that should be performed in all patients with suspected acute pancreatitis.
— Magnetic resonance imaging (MRI) is one of the most important imaging procedures for diagnosing acute pancreatitis and its intraperitoneal complications.
— Computed tomography (CT) is also one of the most important imaging procedures for diagnosing acute pancreatitis and its intraabdominal complications. CT should be performed when a diagnosis of acute pancreatitis cannot be established on the basis of the clinical findings, results of blood and urine tests, or US, or when the etiology of the pancreatitis is unknown.
— When acute pancreatitis is suspected, chest and abdominal X-ray examinations should be performed to determine whether any abnormal findings caused by acute pancreatitis are present.
— Because the etiology of acute pancreatitis can have a crucial influence on both the treatment policy and severity assessment, it should be evaluated promptly and accurately. It is particularly important to differentiate between gallstone-induced acute pancreatitis, which requires treatment of the biliary system, and alcohol-induced acute pancreatitis, which requires a different form of treatment.
Similar content being viewed by others
Clinical questions
-
CQ1.
Are clinical symptoms and signs useful in diagnosing acute pancreatitis?
-
CQ2.
Which pancreatic enzymes should be measured to diagnose acute pancreatitis?
-
CQ3.
What is the optimal examination for diagnosing acute pancreatitis?
-
CQ4.
Is US effective in diagnosing acute pancreatitis?
-
CQ5.
Is MRI effective in diagnosing acute pancreatitis?
-
CQ6.
Is CT effective in diagnosing acute pancreatitis?
-
CQ7.
Are plain X-ray examinations useful in diagnosing acute pancreatitis?
-
CQ8.
Is the etiology of a specific case of acute pancreatitis necessary for its diagnosis?
Introduction
The diagnosis of acute pancreatitis has been based on the clinical manifestations and results of bloodbiochemistry tests, but there are few common criteria that strictly specify the parameters to be used in diagnosis.
The criteria currently used to diagnose acute pancreatitis in Japan were originally developed by the Research Group for Intractable Diseases and Refractory Pancreatic Diseases, which was sponsored by the Japanese Ministry of Health and Welfare (now the Japanese Ministry of Health, Labour, and Welfare). The Research Group states that acute pancreatitis should be diagnosed if the patient presents with at least two of the following three criteria: (1) acute abdominal pain and tenderness in the upper abdomen; (2) elevated levels of pancreatic enzymes in blood, urine, or ascitic fluid; and (3) the presence of abnormal imaging findings in the pancreas that are associated with acute pancreatitis. When a diagnosis is made on this basis, other pancreatic diseases and acute abdomen can be ruled out.
In Japan, many surgeons and physicians specializing in digestive system diseases and emergency medicine are familiar with abdominal ultrasonography (US) and perform it routinely. Magnetic resonance imaging (MRI) is less popular than X-rays or computed tomography (CT) scanning and is not a routine procedure in emergency examinations for abdominal diseases.
The purpose of this article is to review the conventional criteria and, in particular, the various methods of diagnosis based on pancreatic enzyme values, with the aim of improving the quality of the diagnosis of acute pancreatitis and of formulating common, internationally agreed upon criteria.
Diagnostic criteria
Clinical symptoms and signs
Clinical question (CQ) 1. Are clinical symptoms and signs useful in diagnosing acute pancreatitis?
It is essential to interview all patients (including those with consciousness disorders or who are in a state of shock), take their medical histories, and perform a physical examination (Recommendation A)
Abdominal pain, pain radiating to the back, anorexia, fever, nausea and vomiting, and decreased bowel sounds are frequent manifestations of acute pancreatitis (Tables 1 and 2) (Level 4).1,2 However, these features are not specific to acute pancreatitis, and when a patient presents with these manifestations, acute pancreatitis must be differentiated from other acute abdominal diseases. Acute pancreatitis accounts for 2% to 3% of all acute abdominal diseases (Level 2b, unknown)3,4 and in a very few patients there is no abdominal pain (Level 2b).5
Acute pancreatitis is sometimes manifested by discoloration of the skin, such as Grey Turner’s sign (on the lateral abdominal wall), Cullen’s sign (around the navel), and Fox’s sign (over the lower portion of the inguinal ligament). However, because these signs appear in only 3% (Level 2b)6 of patients, and because they are also observed in patients with other diseases (Level 4)7 and are often seen 48 to 72 h after the onset of pancreatitis, their diagnostic significance is low.
Blood and urine tests
Blood lipase
CQ2. Which pancreatic enzymes should be measured to diagnose acute pancreatitis?
When making a diagnosis of acute pancreatitis or a differential diagnosis from other diseases, the blood lipase level is the best pancreatic enzyme parameter, even better than the total blood amylase level (Recommendation A)
Comparisons of measurements of various pancreatic enzymes to detect the presence of acute pancreatitis (Level 2a)8 have shown that the blood lipase level is almost as sensitive as the total blood amylase level and has better specificity (Tables 3 and 4).9,10
According to Apple et al.,8 the sensitivity and specificity of blood lipase in the diagnosis of acute pancreatitis are 85% to 100% and 84.7% to 99.0% (Level 2a),8 respectively. The blood lipase value is more sensitive than blood amylase (Levels 2b-4)11–13 and provides diagnostic capability similar to that of blood P-amylase (Level 2b).13 Blood lipase is considered a valuable diagnostic tool, because abnormally high values persist for longer than abnormal blood amylase levels (Level 2b),14 and it is more sensitive in terms of detecting the presence of acute alcohol-induced pancreatitis. The combined use of blood amylase and blood lipase levels (Level 2a)8 does not facilitate the diagnosis of acute pancreatitis.
The above findings lead to the conclusion that the blood lipase level is an important indicator in the diagnosis of acute pancreatitis and that the measurement of the blood lipase level should be given top priority. Measurement of the lipase level is of primary importance when the blood amylase level of a patient suspected of having acute pancreatitis is normal.
Blood amylase (blood total amylase)
CQ3. What is the optimal examination for diagnosing acute pancreatitis?
Identifying an increase in the level of pancreatic enzymes in the blood is a pivotal factor in the diagnosis of acute pancreatitis (Recommendation A)
When the cutoff blood amylase level is set at the upper limit of normal, it has a sensitivity of 91.7% to 100% and a specificity of 71.6% to 97.6% for the diagnosis of acute pancreatitis. If the cutoff level is set higher, specificity improves, but sensitivity declines. When the cutoff level is set at 1000 IU/l, specificity improves to 100%, but sensitivity declines to 60.9% (Levels 2a-4; Table 5).9,11,16–19 Sensitivity declines because (1) the blood amylase level does not rise as much in many patients with chronic alcoholic pancreatitis with acute exacerbations as it does in patients with acute pancreatitis (Level 2b)12,20 and (2) since the elevated blood amylase level declines almost immediately and is maintained for a shorter time than are other elevated pancreatic enzyme levels, the level must be measured soon after the onset (Levels 3b-4).21,22 The blood amylase level seldom rises in acute pancreatitis caused by hyperlipidemia (Level 3b).23 Because many other diseases besides pancreatitis are associated with hyperamylasemia (Table 6; Level 2a),8 it is necessary to measure extrapancreatic enzymes with high specificity for pancreatitis in order to make a proper differential diagnosis of pancreatitis. If the blood enzyme value and/or imaging findings do not allow for a diagnosis of acute pancreatitis in a patient with ascites, the amylase level in the ascitic fluid may be useful in making the diagnosis. However, it is not usually very useful, because the amylase level in the ascitic fluid sometimes increases in other diseases, including alimentary tract perforation.
P-amylase (amylase isozyme)
The blood P-amylase level is considered useful in the differential diagnosis of hyperamylasemia, and, while one report claimed it could identify 83% of patients (19/23) with hyperamylasemia independent of pancreatic disease (Level 4),24 others suggest a capability of only 20% to 44% (Levels 3b-4).16,19 There is a report describing the blood P-amylase level as a useful indicator, because the abnormally high level is maintained for longer than are the abnormal blood amylase levels in acute pancreatitis (Levels 3b),25 but another report showed that the blood P-amylase level did not improve sensitivity or specificity (Level 2b).17 The diagnostic value of the P-amylase level for acute pancreatitis requires further study.
Blood elastase-1 and other pancreatic enzymes
Clinically measurable extrapancreatic enzymes can be roughly classified into blood and urine amylase, Pamylase (amylase isozyme), and serum lipase, whose enzymatic activity is measured by an enzyme-chemical method; and serum elastase-1, serum trypsin, and serum phospholipase A2 (PLA2), whose antigen levels are measured immunologically. Because the immunological measurements require a lot of time, it is difficult to use them as a routine procedure for the diagnosis of acute pancreatitis. A latex agglutination method has enabled the rapid, convenient measurement of the serum elastase-1 level. Elastase-1 has the advantage of maintaining an abnormally high value for longer than the levels of other pancreatic enzymes (Level 3b),26,27 although the ability to diagnose or assess the severity of acute pancreatitis (Level 2b)28 was not improved by the combined use of the serum elastase-1 and blood amylase levels.
Trypsin is a key enzyme present at the onset of acute pancreatitis, but its activity cannot be measured, because it is too rapidly inactivated by protease inhibitors in the blood, and therefore the quantity of the antigen should be measured immunologically. Blood trypsin has high sensitivity for the diagnosis of acute pancreatitis (Level 2b).23,29 The blood PLA2 level rises markedly in acute pancreatitis and is correlated with the severity (Levels 3b-4).30,31 Qualitative evaluation of urine trypsinogen-2 with test paper to determine its rate of positivity in acute pancreatitis has shown that it has a diagnostic ability similar to that of lipase, and it is expected to be useful in early diagnosis (Levels 3b-4).32,33
Imaging examinations
Ultrasonography (US)
CQ4. Is US effective in diagnosing acute pancreatitis?
Ultrasonography (US) is one of the diagnostic procedures that should be performed first in all patients suspected of having acute pancreatitis (Recommendation A)
Ultrasonography (US) is capable of identifying pancreatic enlargement and inflammatory changes near the pancreas, and it may be useful in diagnosing acute pancreatitis. Although, in severe cases, visualization of the pancreas and peripancreatic tissue may be impaired by gas in the intestinal tract (Levels 1b-2b),34,35 the visualization rate is 62% to 90% for the pancreas, 100% for the peripancreatic tissue in the anterior paranephric cavity, 90% in the cavity of the lesser omentum, and 65% in the mesentery (Levels 1b-2b).34,35 Ultrasonography may also visualize abnormal findings associated with the etiology and morbidity of acute pancreatitis, such as ascites, gallstones, and cholangiectasis. It is particularly important to check for the presence of cholecholithiasis and cholangiectasis when judging whether endoscopic sphincterotomy for gallstone pancreatitis is required. It is desirable to examine patients repeatedly, using US, even when no gallstones are detected by the initial examination. US is also useful for screening for comorbidities such as aneurysms.
Magnetic resonance imaging (MRI)
CQ5. Is MRI effective in diagnosing acute pancreatitis?
MRI is one of the most important imaging procedures for the diagnosis of acute pancreatitis and its intraabdominal complications (Recommendation B)
MRI scanning visualizes pancreatic enlargement and the inflammatory changes around the pancreas (Level 2c)37 and can distinguish the intestinal tract from the necrotic part of the pancreas. Gadolinium-DTPA (Gd-DTPA)-enhanced MRI can visualize foci of pancreatic necrosis (Level 2b).38 MRI accurately depicts the state of necrosis, the main pancreatic ducts, and the extent of inflammation, and it has more value than CT (Levels 2b-3c).39,40 MRI scanning has the advantage of no X-ray exposure. However, because MRI takes much longer than CT scanning and requires the removal of all metal objects (such as respirators and transfusion pumps) before the examination, it is not routinely used to diagnose acute pancreatitis in Japan, where the system for MRI use is not yet adequate. However, magnetic resonance cholangiopancreatography (MRCP) is often required to identify the etiology of acute pancreatitis, such as cholecholithiasis (Level 4)41 and abnormal pancreaticocholedochal junction (abnormal junction of the pancreatobiliary ducts; Level 4).42 MRI scanning can be performed earlier than CT, because it requires no operation of the duodenal papilla and there is no risk of aggravating acute pancreatitis. Although MRCP is noninvasive, it has the disadvantages of less clear imaging than endoscopic retrograde cholangiopancreatography (ERCP) and impaired visualization due to peripancreatic fluid collection.
Computed tomography (CT)
CQ6. Is CT effective in diagnosing acute pancreatitis?
CT is one of the most important imaging procedures for the diagnosis of acute pancreatitis and its intraabdominal complications. CT should be performed when the diagnosis of acute pancreatitis cannot be established on the basis of the clinical findings and the results of blood and urine tests and US, or when the etiology of the pancreatitis is unknown (Recommendation B)
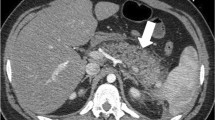
CT is unaffected by the adipose tissue in the abdominal wall and inside the abdominal cavity, and it provides clear local images (Level 1b).34 CT findings useful for the diagnosis of acute pancreatitis include an enlarged pancreas, inflammatory change around the pancreas, fluid collections, uneven density of the pancreatic parenchyma, and traumatic disruption of the pancreas (Figs. 1, 2, and 3). Gas patterns visualized inside and around the pancreas are often due to fistula formation with the intestinal tract and infection by gas-forming anaerobes (Level 1c).36
CT scanning allows for the differentiation of acute pancreatitis from other intraabdominal diseases, such as perforation caused by a gastroduodenal ulcer, and it allows the diagnosis of comorbidities in intraabdominal organs and complications of pancreatitis; it is also an important procedure for assessing the severity of acute pancreatitis and selecting a treatment plan. CT scanning is especially needed in severe acute pancreatitis, where adequate information cannot be obtained by US because of abdominal pain and the complication of ileus.
Plain X-rays
CQ7. Are plain X-ray examinations useful in diagnosing acute pancreatitis?
When acute pancreatitis is suspected, chest and abdominal X-ray examinations should be performed to check for the presence of any abnormal findings caused by acute pancreatitis (Recommendation A)
Abdominal X-ray examinations in acute pancreatitis visualize ileus, localized sentinel loop signs in the left upper abdomen, enlarged duodenal loops and gas collections, colon cutoff signs in the right colon, retroperitoneal gas collection, calcified gallstones, and pancreatolithiasis.
Chest X-rays visualize pleural effusion, acute respiratory distress syndrome (ARDS), and pneumonia. None of these findings, however, are specific enough to make a diagnosis of acute pancreatitis (level 4).44 X-ray examinations are necessary, however, to evaluate the clinical course of acute pancreatitis and to differentiate acute pancreatitis from other diseases, such as alimentary tract perforation.
Search for the etiology
CQ8. Is the etiology of a specific case of acute pancreatitis necessary for its diagnosis?
The etiology of acute pancreatitis may have a crucial impact on treatment policy as well as the severity assessment, and it should be determined promptly and accurately. It is particularly important to differentiate acute gallstone pancreatitis, which requires treatment of the biliary system, from acute alcoholic pancreatitis, which requires a different form of treatment (Recommendation A)
Abdominal US should be performed immediately with the start of treatment in order to detect the presence of abnormal findings associated with the etiology of acute pancreatitis, such as gallstones or dilated bile ducts.
If acute gallstone pancreatitis is accompanied by jaundice, liver disorders, or cholangiectasis, and where cholecholithiasis is suspected, ERCP is required immediately after the onset, but it should be performed only for the purpose of endoscopic treatment, sphincterotomy, and biliary drainage.
ERCP should be performed in patients with acute gallstone pancreatitis who are strongly suspected of having gallstones, but only for the purposes of determining etiology and performing endoscopic treatment. ERCP has several risk factors (level 2b).44 Because ERCP may exacerbate the inflammation at the onset of acute pancreatitis, it should be performed only for limited indications. The guidelines of the British Society of Gastroenterology recommend the performance of ERCP in patients with jaundice, liver disorders, or cholangioectasis, and in those who are strongly suspected of having cholecholithiasis and have had repeated attacks of pancreatitis.45 Patients with repeated attacks of pancreatitis may have anatomical disorders, such as malfusion of the biliary ducts or abnormal junction of the pancreatobiliary ducts, or they may have a tumor or choledocholithiasis. Because such features are difficult to visualize using other procedures, it is recommended that ERCP be performed as a standby procedure to differentiate the etiology of these disorders and complications.45
There is a report claiming that endoscopic US (EUS) can identify cholecholithiasis in 77.8% of patients whose etiology has not been identified by blood tests, US, and CT scanning (level 2b).46 EUS is indicated in any patient with severe acute pancreatitis in whom choledocholithiasis is strongly suspected, but it should be performed only after adequate evaluation of the patient’s general condition. ERCP should be performed without delay. Cases in which cholecholithiasis cannot be diagnosed by extracorporeal US are a good indication for EUS, after the attack subsides.
References
P Malfertheiner TP Kemmer (1991) ArticleTitleClinical picture and diagnosis of acute pancreatitis Hepatogastroenterology 38 97–100 Occurrence Handle1:STN:280:DyaK3MzhtVSguw%3D%3D Occurrence Handle1855780
JP Corsetti DA Arvan (1999) Acute pancreatitis ER Black DR Bordley TG Tape RJ Panzer (Eds) Diagnostic strategies for common medical problems EditionNumber2nd ed. American College of Physicians Philadelphia 205
F de Dombal (1979) ArticleTitleAcute abdominal pain. An OMGE survey Scand J Gastroenterol 56 (Suppl) 14 29–43
FT de Dombal (1991) Diagnosis of acute abdominal pain EditionNumber2nd ed. Churchill Livingstone London 19–30
G Read JM Braganza HT Howat (1976) ArticleTitlePancreatitis: a retrospective study Gut 17 945–52 Occurrence Handle10.1136/gut.17.12.945 Occurrence Handle1:STN:280:DyaE2s7hslWksQ%3D%3D Occurrence Handle1017714
AP Dickson CW Imrie (1984) ArticleTitleThe incidence and prognosis of body wall ecchymosis in acute pancreatitis Surg Gynecol Obstet 159 343–7 Occurrence Handle1:STN:280:DyaL2M%2FhslSqsQ%3D%3D Occurrence Handle6237447
J Bem EL Bradley SuffixIII (1998) ArticleTitleSubcutaneous manifestations of severe acute pancreatitis Pancreas 16 551–5 Occurrence Handle1:STN:280:DyaK1c3lvVOltA%3D%3D Occurrence Handle9598819 Occurrence Handle10.1097/00006676-199805000-00015
F Apple P Benson L Preese S Eastep L Bilodeau G Heiler (1991) ArticleTitleLipase and pancreatic amylase activities in tissues and in patients with hyperamylasemia Am J Clin Pathol 96 610–4 Occurrence Handle1:STN:280:DyaK38%2FlvVygug%3D%3D Occurrence Handle1719798
N Agarwal CS Pitchumoni AV Sivaprasad (1990) ArticleTitleEvaluating tests for acute pancreatitis Am J Gastroenterol 85 356–66 Occurrence Handle1:STN:280:DyaK3c3isV2iuw%3D%3D Occurrence Handle2183590
HJ Thomson PO Obekpa AN Smith WG Brydon (1987) ArticleTitleDiagnosis of acute pancreatitis: a proposed sequence of biochemical investigations Scand J Gastroenterol 22 719–24 Occurrence Handle10.3109/00365528709011149 Occurrence Handle1:STN:280:DyaL1c%2FhslyhsQ%3D%3D Occurrence Handle2443962
AG Nordestgaard SE Wilson RA Williams (1988) ArticleTitleCorrelation of serum amylase levels with pancreatic pathology and pancreatitis etiology Pancreas 3 159–61 Occurrence Handle10.1097/00006676-198804000-00008 Occurrence Handle1:STN:280:DyaL1c3jsVCmtA%3D%3D Occurrence Handle2453872
MD Levitt SG Johnson (1978) ArticleTitleIs the CAm/CCr ratio of value for the diagnosis of pancreatitis? Gastroenterology 75 118–9 Occurrence Handle1:CAS:528:DyaE1cXlt1Gltrk%3D Occurrence Handle95719
SL Orebaugh (1994) ArticleTitleNormal amylase levels in the presentation of acute pancreatitis Am J Emerg Med 12 21–4 Occurrence Handle10.1016/0735-6757(94)90191-0 Occurrence Handle1:STN:280:DyaK2c7hsVSjsQ%3D%3D Occurrence Handle7506911
V Gumaste P Dave G Sereny (1992) ArticleTitleSerum lipase: a better test to diagnose acute alcoholic pancreatitis Am J Med 92 239–42 10.1016/0002-9343(92)90070-R Occurrence Handle10.1016/0002-9343(92)90070-R Occurrence Handle1:STN:280:DyaK387ovFShtA%3D%3D Occurrence Handle1372152
BW Pace S Bank L Wise LC Burson E Borrero (1985) ArticleTitleAmylase isoenzymes in the acute abdomen: an adjunct in those patients with elevated total amylase Am J Gastroenterol 80 898–901 Occurrence Handle1:STN:280:DyaL28%2Fit1Okuw%3D%3D Occurrence Handle2413755
WM Steinberg SS Goldstein ND Davis J Shamma’a K Anderson (1985) ArticleTitleDiagnostic assays in acute pancreatitis. A study of sensitivity and specificity Ann Intern Med 102 576–80 Occurrence Handle1:STN:280:DyaL2M7nt12itg%3D%3D Occurrence Handle2580467
M Ventrucci R Pezzilli P Naldoni L Montone L Gullo (1986) ArticleTitleA rapid assay for serum immunoreactive lipase as a screening test for acute pancreatitis Pancreas 1 320–3 Occurrence Handle10.1097/00006676-198607000-00005 Occurrence Handle1:CAS:528:DyaL2sXhvFWmur4%3D Occurrence Handle3562430
DF Koehler JH Eckfeldt MD Levitt (1982) ArticleTitleDiagnostic value of routine isoamylase assay of hyperamylasemic serum Gastroenterology 82 887–90 Occurrence Handle1:STN:280:DyaL387jvF2ktw%3D%3D Occurrence Handle6174389
PA Clavien J Robert P Meyer F Borst H Hauser F Herrmann et al. (1989) ArticleTitleAcute pancreatitis and normoamylasemia. Not an uncommon combination Ann Surg 210 614–20 Occurrence Handle10.1097/00000658-198911000-00008 Occurrence Handle1:STN:280:DyaK3c%2FlsFChsw%3D%3D Occurrence Handle2479346
JH Eckfeldt JC Kolars MK Elson RB Shafer MD Levitt (1985) ArticleTitleSerum tests for pancreatitis in patients with abdominal pain Arch Pathol Lab Med 109 316–9 Occurrence Handle1:STN:280:DyaL2M7ntlOlsg%3D%3D Occurrence Handle2580501
M Ventrucci R Pezzilli P Naldoni L Plate F Baldoni L Gullo et al. (1987) ArticleTitleSerum pancreatic enzyme behavior during the course of acute pancreatitis Pancreas 2 506–9 Occurrence Handle10.1097/00006676-198709000-00003 Occurrence Handle1:STN:280:DyaL1c%2FktFSitg%3D%3D Occurrence Handle2444967
PP Toskes (1990) ArticleTitleHyperlipidemic pancreatitis Gastroenterol Clin North Am 19 783–91 Occurrence Handle1:STN:280:DyaK3M%2FpvF2htw%3D%3D Occurrence Handle2269517
RJ Vissers RB Abu-Laban DF McHugh (1999) ArticleTitleAmylase and lipase in the emergency department evaluation of acute pancreatitis J Emerg Med 17 1027–37 10.1016/S0736-4679(99)00136-5 Occurrence Handle10.1016/S0736-4679(99)00136-5 Occurrence Handle1:STN:280:DC%2BD3c%2FmtFensw%3D%3D Occurrence Handle10595892
EE Swensson ME King A Malekpour KI Maull (1985) ArticleTitleSerum amylase isoenzyme alterations in acute abdominal conditions Ann Emerg Med 14 421–3 10.1016/S0196-0644(85)80285-7 Occurrence Handle10.1016/S0196-0644(85)80285-7 Occurrence Handle1:STN:280:DyaL2M7nt1ygtw%3D%3D Occurrence Handle2580465
P Leclerc JC Forest (1983) ArticleTitleVariations in amylase isoenzymes and lipase during acute pancreatitis, and in other disorders causing hyperamylasemia Clin Chem 29 1020–3 Occurrence Handle1:STN:280:DyaL3s3gslCrug%3D%3D Occurrence Handle6189637
M Buchler P Malfertheiner W Uhl HG Beger (1986) ArticleTitleDiagnostic and prognostic value of serum elastase-1 in acute pancreatitis Klin Wochenschr 64 1186–91 Occurrence Handle10.1007/BF01728459 Occurrence Handle1:STN:280:DyaL2s7htlOqtA%3D%3D Occurrence Handle3643349
B Flamion M Delhaye Z Horanyi A Delange H Demanet M Quenon et al. (1987) ArticleTitleComparison of elastase-1 with amylase, lipase, and trypsin-like immunoreactivity in the diagnosis of acute pancreatitis Am J Gastroenterol 82 532–5 Occurrence Handle1:STN:280:DyaL2s3htVSntA%3D%3D Occurrence Handle2437792
CE Millson K Charles P Poon J Macfie CJ Mitchell (1998) ArticleTitleA prospective study of serum pancreatic elastase-1 in the diagnosis and assessment of acute pancreatitis Scand J Gastroenterol 33 664–8 Occurrence Handle10.1080/00365529850171963 Occurrence Handle1:STN:280:DyaK1czjt1ejtg%3D%3D Occurrence Handle9669641
M Ventrucci R Pezzilli L Gullo L Plate G Sprovieri L Barbara (1989) ArticleTitleRole of serum pancreatic enzyme assays in diagnosis of pancreatic disease Dig Dis Sci 34 39–45 10.1007/BF01536152 Occurrence Handle10.1007/BF01536152 Occurrence Handle1:STN:280:DyaL1M%2FptVOrtw%3D%3D Occurrence Handle2463138
T Schroder M Lempinen E Kivilaakso P Nikki (1982) ArticleTitleSerum phospholipase A2 and pulmonary changes in acute fulminant pancreatitis Resuscitation 10 79–87 10.1016/0300-9572(82)90015-6 Occurrence Handle10.1016/0300-9572(82)90015-6 Occurrence Handle1:STN:280:DyaL3s%2Fpt1Cltg%3D%3D Occurrence Handle6294771
J Nishijima M Okamoto M Ogawa G Kosaki T Yamano (1983) ArticleTitlePurification and characterization of human pancreatic phospholipase A2 and development of a radioimmunoassay J Biochem (Tokyo) 94 137–47 Occurrence Handle1:CAS:528:DyaL3sXks1Knt7s%3D
EA Kemppainen JI Hedstrom PA Puolakkainen VS Sainio RK Haapiainen V Perhoniemi et al. (1997) ArticleTitleRapid measurement of urinary trypsinogen-2 as a screening test for acute pancreatitis N Engl J Med 19 1788–93 Occurrence Handle10.1056/NEJM199706193362504
YT Chen CC Chen SS Wang FY Chang SD Lee (2005) ArticleTitleRapid urinary trypsinogen-2 test strip in the diagnosis of acute pancreatitis Pancreas 30 243–7 Occurrence Handle10.1097/01.mpa.0000153618.48137.ef Occurrence Handle1:CAS:528:DC%2BD2MXjsVyit7k%3D Occurrence Handle15782102
W Silverstein MB Isikoff MC Hill J Barkin (1981) ArticleTitleDiagnostic imaging of acute pancreatitis: prospective study using CT and sonography AJR Am J Roentgenol 137 497–502 Occurrence Handle1:STN:280:DyaL38%2FitVOrsw%3D%3D Occurrence Handle7025598
RB Jeffrey SuffixJr FC Laing VW Wing (1986) ArticleTitleExtrapancreatic spread of acute pancreatitis: new observations with real-time US Radiology 159 707–11 Occurrence Handle3517954
ES Alexander RA Clark MP Federle (1982) ArticleTitlePancreatic gas: indication of pancreatic fistula AJR Am J Roentgenol 139 1089–93 Occurrence Handle1:STN:280:DyaL3s%2FntFeluw%3D%3D Occurrence Handle6983251
A Piironen R Kivisaari E Kemppainen P Laippala AM Koivisto VP Poutanen et al. (2000) ArticleTitleDetection of severe acute pancreatitis by contrast-enhanced magnetic resonance imaging Eur Radiol 10 354–61 10.1007/s003300050055 Occurrence Handle10.1007/s003300050055 Occurrence Handle1:STN:280:DC%2BD3c7jtV2hsA%3D%3D Occurrence Handle10663768
A Saifuddin J Ward J Ridgway AG Chalmers (1993) ArticleTitleComparison of MR and CT scanning in severe acute pancreatitis: initial experiences Clin Radiol 48 111–6 Occurrence Handle10.1016/S0009-9260(05)81083-9 Occurrence Handle1:STN:280:DyaK2c3ntlChug%3D%3D Occurrence Handle8004888
M Hirota Y Kimura T Ishiko T Beppu Y Yamashita M Ogawa (2002) ArticleTitleVisualization of the heterogeneous internal structure of so-called “pancreatic necrosisȝ by magnetic resonance imaging in acute necrotizing pancreatitis Pancreas 25 63–7 10.1097/00006676-200207000-00015 Occurrence Handle10.1097/00006676-200207000-00015 Occurrence Handle12131773
M Arvanitakis M Delhaye V De Maertelaere M Bali C Winant E Coppens et al. (2004) ArticleTitleComputed tomography and magnetic resonance imaging in the assessment of acute pancreatitis Gastroenterology 126 715–23 10.1053/j.gastro.2003.12.006 Occurrence Handle10.1053/j.gastro.2003.12.006 Occurrence Handle14988825
DJ Lomas PWP Bearcroft AE Gimson (1999) ArticleTitleMR cholangiopancreatography: prospective comparison of a breath-hold 2D projection technique with diagnostic ERCP Eur Radiol 9 1411–7 10.1007/s003300050859 Occurrence Handle10.1007/s003300050859 Occurrence Handle1:STN:280:DyaK1MzptVSntQ%3D%3D Occurrence Handle10460385
S Hirohashi R Hirohashi H Uchida M Akira T Itoh E Haku et al. (1997) ArticleTitlePancreatitis: evaluation with MR cholangiopancreatography in children Radiology 203 411–5 Occurrence Handle1:STN:280:DyaK2s3mvVOnug%3D%3D Occurrence Handle9114096
C Dervenis CD Johnson C Bassi E Bradley CW Imrie MJ McMahon et al. (1999) ArticleTitleDiagnosis, objective assessment of severity, and management of acute pancreatitis. Santorini Consensus Conference Int J Pancreatol 25 195–210 Occurrence Handle1:STN:280:DyaK1Mzot1OqsQ%3D%3D Occurrence Handle10453421
GN Stein MH Kalser NN Sarian A Finkelstein (1959) ArticleTitleAn evaluation of the roentgen changes in acute pancreatitis: correlation with clinical findings Gastroenterology 36 354–61 Occurrence Handle1:STN:280:DyaG1M%2FmvFOmug%3D%3D Occurrence Handle13640153
S Loperfido G Angelini G Benedetti F Chilovi F Costan F De Berardinis et al. (1998) ArticleTitleMajor early complications from diagnostic and therapeutic ERCP: a prospective multicenter study Gastrointest Endosc 48 1–10 10.1016/S0016-5107(98)70121-X Occurrence Handle10.1016/S0016-5107(98)70121-X Occurrence Handle1:STN:280:DyaK1czkslOquw%3D%3D Occurrence Handle9684657
InstitutionalAuthorNameBritish Society of Gastroenterology (1998) ArticleTitleUnited Kingdom guidelines for the management of acute pancreatitis Gut 42 IssueIDSuppl 2 S1–13
CL Liu CM Lo JKF Chan RTP Poon ST Fan (2000) ArticleTitleEUS for detection of occult cholelithiasis in patients with idiopathic pancreatitis Gastrointest Endosc 51 28–32 10.1016/S0016-5107(00)70382-8 Occurrence Handle10.1016/S0016-5107(00)70382-8 Occurrence Handle1:STN:280:DC%2BD3c%2Fpt1Oqsw%3D%3D Occurrence Handle10625791
Author information
Authors and Affiliations
About this article
Cite this article
Koizumi, M., Takada, T., Kawarada, Y. et al. JPN Guidelines for the management of acute pancreatitis: diagnostic criteria for acute pancreatitis. J Hepatobiliary Pancreat Surg 13, 25–32 (2006). https://doi.org/10.1007/s00534-005-1048-2
Issue Date:
DOI: https://doi.org/10.1007/s00534-005-1048-2